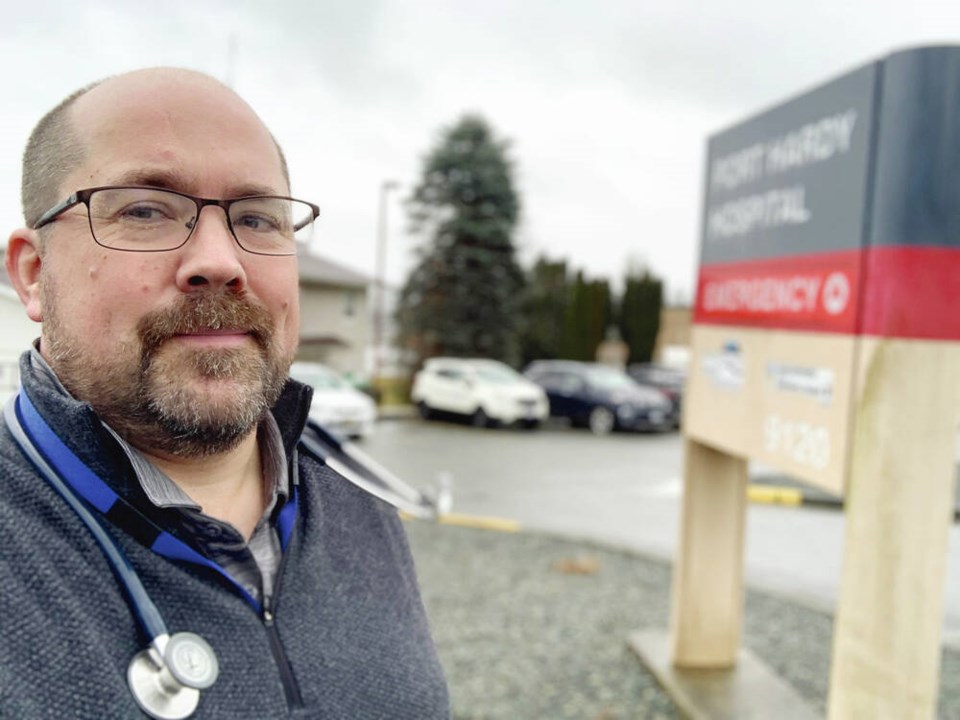
The president of the Doctors of B.C. is in Port Hardy this weekend to work three emergency shifts as the hospital struggles with a staffing shortage.
Dr. Joshua Greggain, who lives in Victoria, volunteered to take ER shifts Saturday through Monday at Port Hardy Hospital to assist with an acute staffing shortage that worsened when one physician lost his ER privileges this month.
Greggain said physicians are needed as locums in the community for the next three to six months to help stabilize the situation. He wants to hear from local health-care staff while he’s in the community. “There’s a level of desperation in the nurses, the physicians, the entire team, where there just simply aren’t enough people here to provide their service.”
He said some physicians are working 14 ER shifts a month to try and keep the doors open, and “they’re struggling to even do that during the daytime.”
Last month, as staffing shortages worsened, Island Health temporarily closed Port Hardy and Cormorant Hospital emergency departments overnight.
Port McNeill Hospital, about 40 kilometres from Port Hardy, is the only acute-care hospital ER in the region open 24 hours a day.
B.C. Health Minister Adrian Dix said $30 million in new operating and capital funding recently provided for the Mount Waddington region includes incentives for staff retention and referral, incentives to travel to fill shifts, renovations to staff accommodations, and the hiring of 10 additional protection officers to improve safety.
The funding will also prioritize a new daily shuttle between hospitals for patients and staff, a mobile CT diagnostic service, four new long-term care beds at the Port Hardy Hospital, hospital upgrades, and increased support for home-health, mental health, substance use, and home support services.
Greggain, who has practised rural family medicine since 2005, including 14 years full-time in Hope, said the health-care workers he’s hearing from in the north Island feel the new funding isn’t enough without more people to do the work.
Labour shortages aren’t just being felt in emergency wards but in maternity services, medical assistance in dying, long term care facilities and outreach services, said Greggain.
Eighteen months ago, the same doctors and nurses felt they had enough hands to do the work “and now they’re absolutely desperate,” he said.
When a physician has to do three jobs — be in the hospital, provide long-term care and work in a clinic — there can be a sense of always failing to do one’s best, said Greggain, who does mostly rural locums across the province, as well as the occasional shift at the downtown Victoria Urgent and Primary Care Centre.
“I think there’s a multitude of communities across the province that are in a similar spot.”
A nurse manager told him Friday that everyone from physicians to nurses, nurse practitioners, and lab and X-ray technicians is needed.
There’s a long-term strategy for how the province can attract more physicians and nurses, Greggain said, “but right now, in February 2023, it feels particularly desperate in Port Hardy, which is why I think they’re looking for acute and urgent solutions to help.”
>>> To comment on this article, write a letter to the editor: [email protected]